During the long road to healing, Charlene and Savannah spent plenty of quality time together.
Top Doctors
Becoming a Patient Advocate
Charlene Waszczuk went from Christmas shopping one day to fighting for her life at Mercy Springfield’s Intensive Care Unit the next. Her daughter recounts the experience and gives a few tips if you ever find yourself in a similar situation.
By Savannah Waszczuk
May 2018

Ask a group of kids to recite their worst fears, and you’ll hear a slew of common answers. Snakes. Spiders. Sharks. The dark. But not me. Among a sea of 7-year-olds, my worst fear stood out: I was afraid of losing my mom.
Fast forward 25 years, and all is the same. Now I’m 32, but I don’t have kids or a husband of my own. My mom is still the No. 1 person in my life—the one I always text before bed and call on my way home from work. She’s my listening ear and my personal cheerleader, my shopping buddy and my lifelong Scrabble opponent. My mom is my best friend, and I can’t imagine living without her. That’s why my life changed forever last December 22.
The Morning That Started It All
It was the last day that I had to work before Christmas break, so I was in a great mood despite waking up to gray skies and a cold drizzle. I was about to leave my house when I got a text from Chris, my second-oldest brother: “What in the world is going on with Mom? Cayla tried dropping off the girls, and the house was dark. No one answered the door, and she’s not answering her phone. Something is wrong.”
My heart sank. I immediately panicked as I realized I hadn’t heard from Mom last night or that morning, either. She was supposed to watch my nieces, and she wasn’t even awake. That’s not like her. I ran to my car and began what felt like the longest drive of my life—I was headed to the old hilltop farmhouse where I grew up, and I had no idea what would be waiting for me when I arrived. So many thoughts flooded my brain. Christmas was in three days. I pictured what would be the first Christmas morning of my life where we weren’t all gathered in my parents’ living room. Alternative scenarios forced tears down my cheeks. After half a dozen calls, I finally got in touch with my nephew, Zane, who lived in the home with my brother, my dad and my mom: “Grandmom is coughing up blood and can’t breathe.”
“Christmas was in three days. I pictured what would be the first Christmas morning of my life where we weren’t all gathered in my parents’ living room.”— Savannah Waszczuk
Mom was at 30 percent oxygen by the time we got her to the Mercy emergency room, and her body went into septic shock (a medical condition that affects the body after organs are injured or damaged as a result of a severe infection). She was immediately intubated. We soon learned she also had double pneumonia, a condition that’s bad for anyone, but extra-concerning for someone with her other chronic conditions: COPD, emphysema and a compromised lung due to a severe case of scoliosis. A few hours later we were told she made it to the ER just in time, but her outcome was questionable. They said the next 12 to 24 hours were critical.
My brothers and I sat subdued. We prayed together. We prayed over Mom. We paced the floors. We texted family back east and updated Facebook requesting prayers. Soon we all made a bittersweet walk to the Mercy ICU; each step was weighted with the fear of what might happen next. As days went on, those steps became all too familiar. ICU room No. 6118 became mom’s home for the next 14 days, and each day brought a new set of uncertainties.
Night One
All nights were hard, but night one was among the worst. Mom’s blood pressure was dipping, then spiking. They were uncertain of what infection caused her body to go septic, which meant they didn’t know what antibiotics to use to treat it. Her temperature had risen to more than 105 degrees by 9 p.m. I felt sick to my stomach as I watched her lying lifeless in that stark, dark room, machines breathing for her.
Before I left, I asked the nurses how they’d lower her temperature since they hadn’t been able to so far. The plan was to cover her body in cooling blankets and pump her veins full of Tylenol. I continued asking questions. How do the cooling blankets work? How much Tylenol? When will we know if it’s working? What will we try if it doesn’t? I wrote everything down.
I looked at my dad, who is on a plethora of medications of his own due to a history of mental illness. He was staring down the empty hospital hallway—I knew he was in shock. I then looked at my two brothers, both who love my mom every bit as much as I do but also have two kids of their own to worry about. That’s the moment that I realized that this was my job. I was the one who needed to ask questions and learn about medications. I was the one who needed to connect bridges from nurse to nurse, from therapist to therapist, from doctor to doctor. It was time for me to step up and be my mom’s advocate. As the days continued, I learned that this was far more important than I even knew.
I hated leaving knowing I wouldn’t get a goodnight text that night. I hated it even more when I thought about how I might never talk to my mom again. I didn’t sleep at all. Instead, I prayed. A lot. It was one of the only things that brought me any comfort. Mom’s temperature dropped about a degree and a half every two hours, and it was down to 101 around 4:30 a.m. At 4:45, the ICU nurse called me and told me to get my family there as soon as possible—Mom’s heart was suddenly out of rhythm, and they didn’t know why. She had possibly had an unknown heart attack previously, or she had an unknown, pre-existing problem that quickly became a much bigger problem considering the state of her body. I called my brothers and Dad. After spending what felt like an eternity in Mercy’s sixth floor waiting room, we learned that she had survived this stint. Her heart went into Atrial Fibrillation (AFib), and they had another issue to fix: now they had to find a way to get her heart back into a regular rhythm. After a few scary days, they found the appropriate meds to control it.

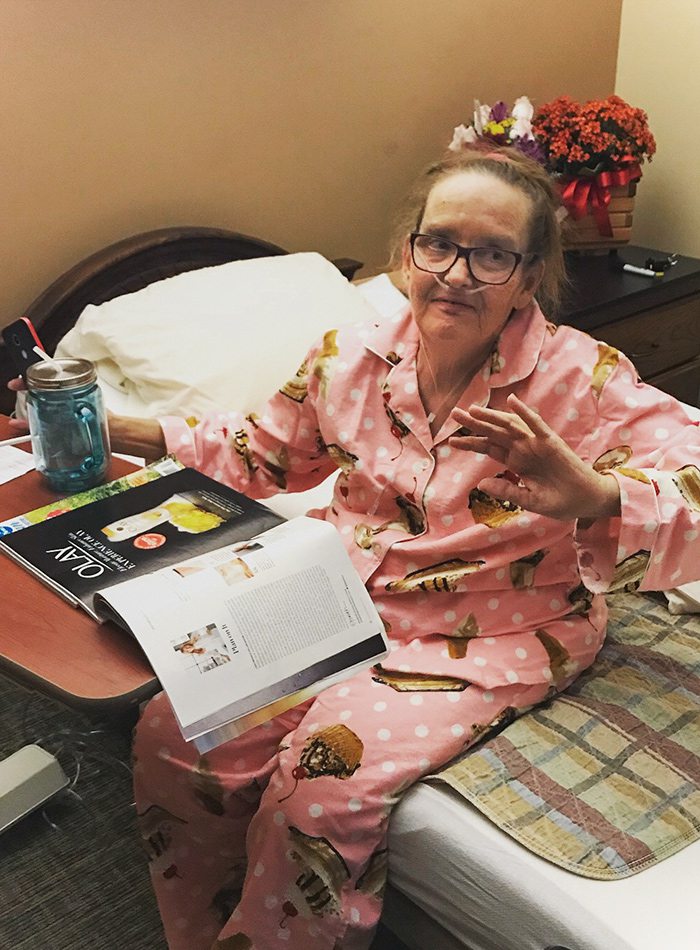
Due to a string of health complications, Charlene Waszczuk almost lost her life. Her daughter, Savannah, learned how to adjust to the stress of living life on the edge.

Savannah and family spent Christmas Eve in the hospital to be near her mom, Charlene.
Learning How to Live Again
My life since that very first night has been a blur. The full story is riddled with multiple events like the heart incident—it has been a journey full of ups and downs and highs and lows. As I write this, we’re at a high point: Mom is finally home after two weeks in the ICU, a week in a regular hospital room and a month at The Maples Health & Rehabilitation Center. Tied to this is another low point—Mom’s home isn’t that same picturesque farmhouse where I grew up anymore. That home burned to the ground two weeks into her stay at The Maples. My dad, nephew and brother all made it out alive, though, and for that, we’re thankful.
People often ask me how I’ve remained so optimistic with all of these things going on. Seeing all of the bad—and having doctor after doctor tell me how lucky we are that my mom is still alive—has made me much more appreciative of all of the good. I’ll never forget the first time Mom squeezed my hand to let me know she could hear my voice. I won’t forget the first time she talked to my brother and me again. I won’t forget when she could drink water again, or when she could swallow food again, or when she could walk again. These things all used to be normal, but now they’re the things I celebrate. Sure, my life changed forever on December 22, but to me, it has become so much more beautiful. Now when Mom and I have an after-work talk or play a lazy Saturday game of Scrabble, I can’t help but think about how these moments were so close to being gone forever. And now they’re happening, day after day. For that, how can I be anything but grateful?
Hospital How-Tos
When a family member becomes critically ill, your life changes in an instant. Here are a few tips for surviving the challenging time and being a health advocate for your loved one.
Ask Questions.
It’s important to understand what’s going on with your loved one, and it’s crucial that you understand the medications they’re taking. Ask lots of questions. I found that many doctors and nurses were happy to explain things to me, and they even broke it down in simpler terms when I needed it.
Write Things Down.
Things change often and happen quickly—especially in the ICU. I took notes during my conversations with medical staff, and I wrote down all of my mom’s medications—this helped make sure I didn’t miss anything and also helped me update my other family members.
Bridge the Gaps.
The doctors and nurses in the Mercy ICU communicated well with each other, but the communication among staff members isn’t quite as involved on the regular hospital room floor or in the rehabilitation center. Each time I met new doctors, nurses or therapists, I updated them on Mom’s case and made sure they knew of her pre-existing conditions (such as her scoliosis, which made a huge difference in the way she could lay or move).
Find Your Strength.
My mom was on the sixth floor of Mercy Springfield, which is also where the hospital’s chapel is located—my family and I recited the rosary together in the chapel daily. I also talked to friends, which helped. Find activities that bring you peace, and try to engage with them each day.
Eat the Pie!
Plenty of people will tell you this (and if you’re like me, it might frustrate you at times), but don’t forget to take care of yourself. My advice on this is to be aware of your limits, but let yourself be at the hospital if you feel you need to be. When you do have an appetite (and if you’re at Mercy Springfield), go down to the cafeteria, and eat the pie—the mint chocolate was my favorite, but all were delicious!
Top Doctors
Looking for the perfect healthcare provider? 417 Magazine's annual Top Doctors list features winning physicians in medical and surgical specialties throughout 417-land. These physicians were selected by their peers in the local medical community who voted for them in our Top Doctors survey.











