Top Doctors
Fighting the Opioid Crisis in Southwest Missouri
CoxHealth is on a mission to bring community partners together to combat the rise of opioid use in the Ozarks.
By Ettie Berneking
Jul 2020
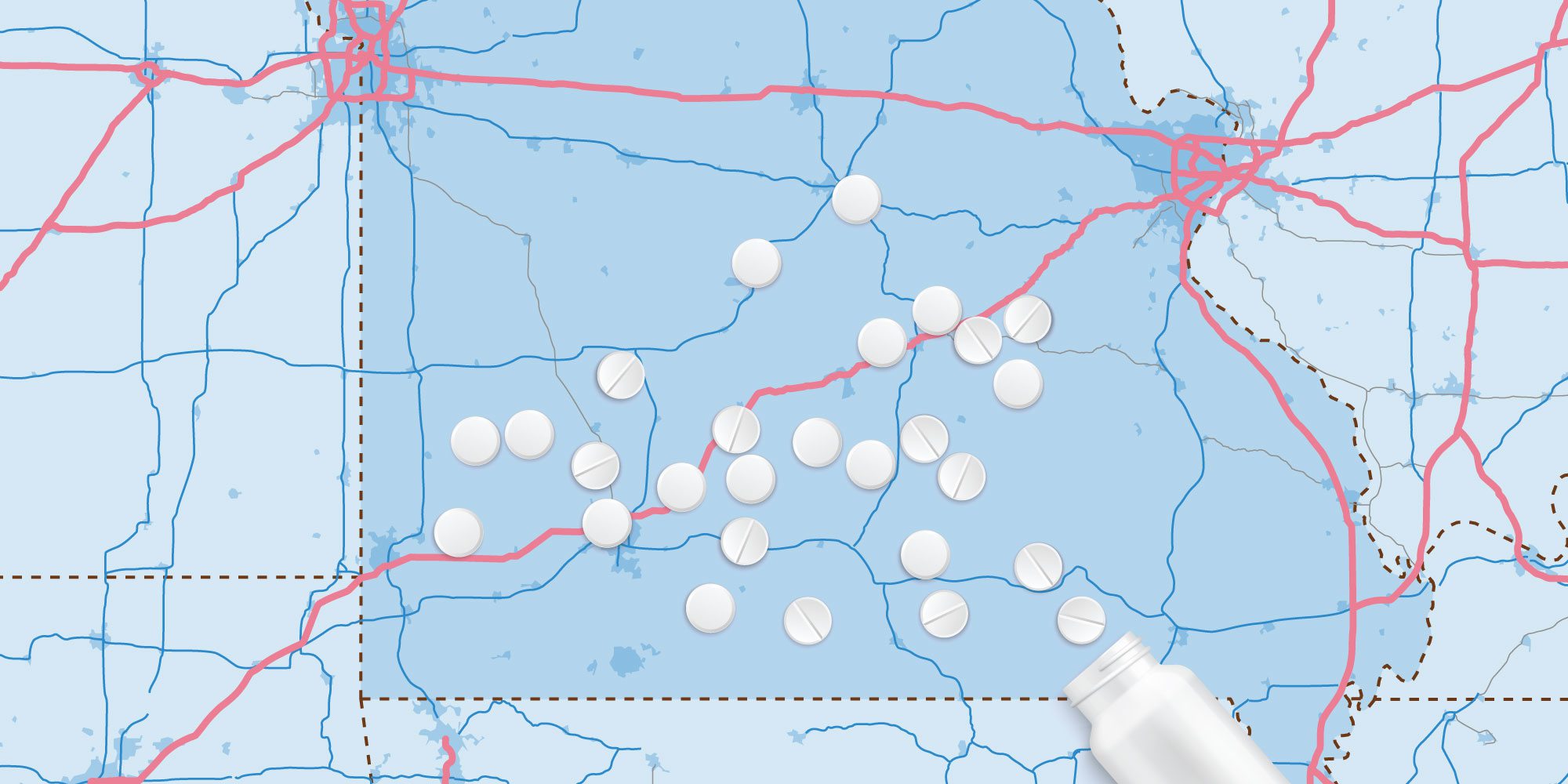
Providing health care to rural communities is a nationwide struggle, but in the Ozarks, that struggle is compounded by the rise of opioid use and overdose deaths. According to the National Institute on Drug Abuse, Missouri saw a 40% increase in deaths involving synthetic opioids such as fentanyl from 2017 to 2018, and southwest Missouri has the third highest overdose death rate per 100,000 at 9.1 as reported by the Missouri Overdose Rescue and Education Project.
“Nationwide, there’s a decrease in opioid use, but in our area, it’s not decreasing,” says Brandi VanAntwerp, grant administrator at CoxHealth Foundation. “This is likely due to two factors—the slow response to increased availability of naloxone and the lack of a statewide Prescription Drug Monitoring Program (PDMP). Missouri is the only state in the country without a PDMP.” So when Cox received a $1 million grant to be used between 2019 and 2022 to combat substance use disorder and opioid use disorder and help with recovery efforts in rural communities, the team at Cox got to work. Their first step was gathering health care partners around the table including the addiction facility Ozark Center in Joplin, Burrell Behavioral Health, the Jordan Valley Community Health Center and CoxHealth Center Branson. Burrell Behavioral Health actually received a $4 million grant from the Substance Abuse and Mental Health Services Administration this past May to make mental health services (including opioid and substance use treatment) affordable for those who need it.
“Nationwide, there’s a decrease in opioid use, but in our area, it’s not decreasing.”— Brandi VanAntwerp, Grant Administrator at CoxHealth Foundation
The final plan for distributing Cox’s grant funding broke down into three categories: prevention of substance abuse, treatment for substance abuse and recovery activities. In total, Cox has teamed up with 15 community partners around Barton, Barry, Lawrence, Stone and Taney counties to help staff, fund and direct opioid prevention and treatment efforts. They’re also working on implementing universal screening so all 15 partners can spot substance abuse in patients before they overdose. VanAntwerp says one of the goals is to create long term community partnerships so health care leaders can continue to fight opioid abuse long after the grant has expired.